Cancer is one of the leading causes of death worldwide, but early detection can significantly improve the chances of successful treatment and survival. Cancer screening is a vital process that can help identify certain types of cancer before symptoms appear, allowing for timely intervention. This preventive approach is essential for reducing the burden of cancer and improving the overall outcomes for patients. In this article, we will explore the importance of cancer screening, when it should be done, and why it plays a crucial role in cancer prevention and treatment.
1. What is Cancer Screening?
Cancer screening involves testing individuals who do not show any symptoms for certain types of cancer, with the goal of detecting cancer at an early, more treatable stage. Screening tests can be performed for various cancers, such as breast cancer, cervical cancer, colorectal cancer, and lung cancer. These tests are designed to detect cancer before it progresses, making it easier to treat and increasing the likelihood of a positive outcome.
While screening tests cannot guarantee prevention or a cure, they can detect cancer at a stage where treatment is more likely to be successful. Regular screenings are especially important for individuals at higher risk of certain types of cancer due to family history, lifestyle, or environmental factors.
2. Why is Cancer Screening Important?
Cancer screening is crucial because it can detect cancers in their early stages, often before symptoms appear. Early-stage cancers are generally more responsive to treatment and may be easier to remove or treat with less invasive procedures. Screening can also help identify precancerous conditions, allowing for preventive measures to be taken before cancer develops.
Some of the main reasons why cancer screening is important include:
- Early Detection: Cancer screening helps identify abnormal cell growth or tumors at an early stage when treatment is most effective. Early detection can lead to better outcomes and higher survival rates.
- Prevention: Certain screenings can detect precancerous changes, which may allow for the removal of abnormal cells before they develop into full-blown cancer.
- Cost-Effectiveness: Treating cancer in its early stages is often more cost-effective than treating advanced cancer. Early-stage cancers require fewer treatments and result in shorter hospital stays.
- Improved Survival Rates: With early detection, the chances of successful treatment and long-term survival increase significantly. For example, the survival rate for breast cancer is much higher when diagnosed early.
- Reduced Mortality: Regular screening has been shown to reduce cancer-related deaths by identifying cancers early, when they are more treatable.
3. When Should Cancer Screening Be Done?
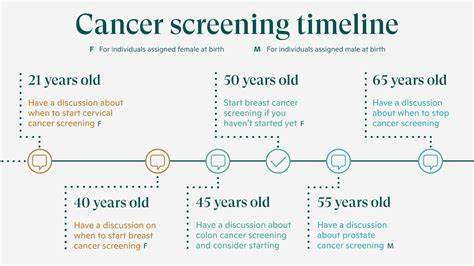
The timing of cancer screenings depends on various factors, including age, gender, family history, and personal risk factors. For individuals with no symptoms and a low risk of cancer, most guidelines recommend starting screening at certain age milestones. For individuals with a higher risk due to family history or genetic predisposition, screening may need to begin earlier or be done more frequently.

Here are the general recommendations for cancer screening:
- Breast Cancer: Women should begin regular mammogram screenings at age 40, with annual or biennial screenings recommended depending on individual risk factors. Women with a family history of breast cancer or genetic mutations such as BRCA may need to begin screenings earlier.
- Cervical Cancer: Women should begin cervical cancer screening (Pap smears) at age 21 and continue every three years until age 29. From age 30 to 65, women may choose to have a Pap smear every three years or a combination of a Pap smear and HPV test every five years. After age 65, women may stop screening if they have had normal results for several years.
- Colorectal Cancer: Adults should begin colorectal cancer screenings at age 45, with the frequency depending on the type of screening test used. For example, a colonoscopy is typically recommended every 10 years, while stool-based tests may be done more frequently.
- Lung Cancer: Lung cancer screening is recommended for individuals aged 55 to 80 who have a history of heavy smoking (at least 30 pack-years) and currently smoke or have quit within the past 15 years. Screening is typically done with low-dose CT scans.
- Prostate Cancer: Men should discuss prostate cancer screening with their doctor starting at age 50, or earlier if they have a family history of prostate cancer. The decision to undergo screening should be based on personal risk factors and the potential benefits and risks of the test.
- Skin Cancer: Regular skin checks are essential for detecting skin cancer, especially for individuals with a high risk of melanoma, such as those with fair skin, a family history of skin cancer, or a history of excessive sun exposure. Self-examination and professional skin exams are recommended annually.
- Ovarian Cancer: While there is no routine screening for ovarian cancer for the general population, women at high risk due to genetic factors or family history should discuss options with their healthcare provider.
It is important to note that these recommendations are general guidelines, and the best screening schedule for an individual should be discussed with their healthcare provider, taking into account their medical history and risk factors.
4. Common Types of Cancer Screening Tests
Several screening tests are used to detect different types of cancer. Some of the most common cancer screenings include:
- Mammography: A mammogram is an X-ray of the breast that can detect early signs of breast cancer, even before symptoms appear. It is one of the most widely used screening tests for women.
- Pap Smear: A Pap smear is a test that collects cells from the cervix to check for abnormalities that could indicate cervical cancer or precancerous changes.
- Colonoscopy: A colonoscopy involves using a long, flexible tube with a camera to examine the colon and rectum for signs of cancer or polyps that could develop into cancer.
- Low-Dose CT Scan: This imaging test is used to screen for lung cancer in individuals at high risk, such as long-term smokers.
- Stool-Based Tests: These tests, such as the fecal occult blood test (FOBT) or fecal immunochemical test (FIT), are used to check for signs of colorectal cancer by detecting hidden blood in stool samples.
- Prostate-Specific Antigen (PSA) Test: A blood test that measures the level of PSA, a protein produced by the prostate. Elevated levels of PSA may indicate prostate cancer, although other conditions can also cause high PSA levels.
- Skin Exams: A skin exam by a dermatologist or self-examination can help detect skin cancer, particularly melanoma.
Each of these tests has its advantages and limitations, and the choice of screening method depends on factors such as the type of cancer, the patient’s risk, and the test’s sensitivity.
5. Challenges and Limitations of Cancer Screening
While cancer screening can be life-saving, it is not without its challenges and limitations. Some of the common issues include:

- False Positives and False Negatives: No screening test is perfect. A false positive may lead to unnecessary follow-up tests and treatments, while a false negative may result in undiagnosed cancer.
- Overdiagnosis: Some cancers detected through screening may never cause symptoms or harm during a person’s lifetime. This can lead to unnecessary treatments and potential side effects.
- Cost and Accessibility: Some individuals may have difficulty accessing or affording regular cancer screenings, which can delay early detection.
- Psychological Impact: The anxiety and stress caused by abnormal screening results or the possibility of a cancer diagnosis can be emotionally taxing for patients.
Despite these limitations, the benefits of cancer screening generally outweigh the risks, particularly for individuals at high risk or those over the recommended age for screenings.
6. Conclusion
Cancer screening is a vital tool in the fight against cancer, offering early detection and a higher likelihood of successful treatment. Regular screenings can help catch cancers before they progress, leading to better outcomes and reduced mortality rates. While it’s essential to follow guidelines for screening based on age, risk, and family history, individuals should also consult with their healthcare provider to create a personalized screening plan. By incorporating cancer screening into regular health check-ups, individuals can take a proactive approach to their health and increase their chances of catching cancer early, improving their overall quality of life.

Leave a Reply